News Details
Varicose veins
- By:
- Posted 1/1/0001 12:00:00 AM
- 0 Comments
- 0 Views
- Rating: 0
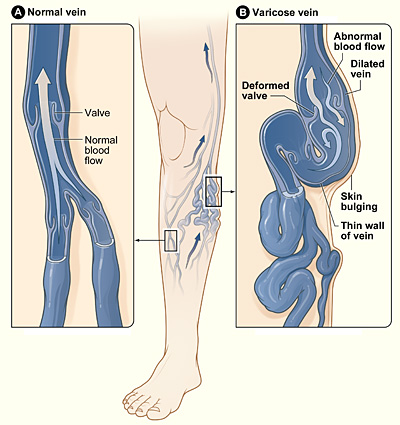
Varicose veins are veins that have become enlarged and tortuous. The term commonly refers to the veins on the leg, although varicose veins can occur elsewhere. Veins have leaflet valves to prevent blood from flowing backwards (retrograde). Leg muscles pump the veins to return blood to the heart, against the effects of gravity. When veins become varicose, the leaflets of the valves no longer meet properly, and the valves do not work. This allows blood to flow backwards and they enlarge even more. Varicose veins are most common in the superficial veins of the legs, which are subject to high pressure when standing. Besides cosmetic problems, varicose veins are often painful, especially when standing or walking. They often itch, and scratching them can cause ulcers. Serious complications are rare. Non-surgical treatments include sclerotherapy, elastic stockings, elevating the legs, and exercise. The traditional surgical treatment has been vein stripping to remove the affected veins. Newer, less invasive treatments, such as ultrasound-guided foam sclerotherapy, radiofrequency ablation and endovenous laser treatment, are slowly replacing traditional surgical treatments. Because most of the blood in the legs is returned by the deep veins, the superficial veins, which return only about 10 per cent of the total blood of the legs, can usually be removed or ablated without serious harm. Varicose veins are distinguished from reticular veins (blue veins) and telangiectasias (spider veins), which also involve valvular insufficiency,[4] by the size and location of the veins. Many patients who suffer with varicose veins seek out the assistance of physicians who specialize in vein care. These physicians are called phlebologists.
Signs and symptoms
- Aching, heavy legs (often worse at night and after exercise).
- Appearance of spider veins (telangiectasia) in the affected leg.
- Ankle swelling.
- A brownish-blue shiny skin discoloration near the affected veins.
- Redness, dryness, and itchiness of areas of skin - termed stasis dermatitis or venous eczema, because of waste products building up in the leg.
- Cramps may develop especially when making a sudden move as standing up.
- Minor injuries to the area may bleed more than normal and/or take a long time to heal.
- In some people the skin above the ankle may shrink (lipodermatosclerosis) because the fat underneath the skin becomes hard.
- Restless legs syndrome appears to be a common overlapping clinical syndrome in patients with varicose veins and other chronic venous insufficiency.
- Whitened, irregular scar-like patches can appear at the ankles. This is known as atrophie blanche.
Complications
Most varicose veins are relatively benign, but severe varicosities can lead to major complications, due to the poor circulation through the affected limb.
- Pain, heaviness, inability to walk or stand for long hours thus hindering work
- Skin conditions / Dermatitis which could predispose skin loss
- Skin ulcers especially near the ankle, usually referred to as venous ulcers.
- Development of carcinoma or sarcoma in longstanding venous ulcers. There have been over 100 reported cases of malignant transformation and the rate is reported as 0.4% to 1%.
- Severe bleeding from minor trauma, of particular concern in the elderly.
- Blood clotting within affected veins. Termed superficial thrombophlebitis. These are frequently isolated to the superficial veins, but can extend into deep veins becoming a more serious problem.
- Acute fat necrosis can occur, especially at the ankle of overweight patients with varicose veins. Females are more frequently affected than males.
Stages
- C0 no visible or palpable signs of venous disease
- C1 telangectasia or reticular veins
- C2 varicose veins
- C3 edema
- C4a skin changes due to venous disorders: pigmentation, eczema
- C4b skin changes due to venous disorders: lipodermatosclerosis, atrophie blanche
- C5 as C4 but with healed ulcers
- C6 skin changes with active ulcers (venous insufficiency ulceration)
Causes
Varicose veins are more common in women than in men, and are linked with heredity. Other related factors are pregnancy, obesity, menopause, aging, prolonged standing, leg injury, abdominal straining, and crossing legs at the knees or ankles. Less commonly, but not exceptionally, varicose veins can be due to other causes, as post phlebitic obstruction and/or incontinence, venous and arteriovenous malformations...
Conservative Treatment
The symptoms of varicose veins can be controlled to an extent with the following:
- Elevating the legs often provides temporary symptomatic relief.
- "Advice about regular exercise sounds sensible but is not supported by any evidence."
- The wearing of graduated compression stockings with variable pressure gradients (Class II or III) has been shown to correct the swelling, nutritional exchange, and improve the microcirculation in legs affected by varicose veins. They also often provide relief from the discomfort associated with this disease. Caution should be exercised in their use in patients with concurrent arterial disease.
- Diosmin/Hesperidine and other flavonoids.
- anti-inflammatory medication such as ibuprofen or aspirin can be used as part of treatment for superficial thrombophlebitis along with graduated compression hosiery – but there is a risk of intestinal bleeding. In extensive superficial thrombophlebitis, consideration should be given to anti-coagulation, thrombectomy or sclerotherapy of the involved vein.
- excessive fear can cause leg fold up, habit like fold up sit, so use normal sit without folding legs, don't fold legs for long time.
The American College of Phlebology (ACP) is a professional organization of physicians and allied health professionals that treat venous disease. Their membership spans 7 continents and 38 countries. To find a provider in your area visit www.phlebology.org or www.healthyveins.org
Active Treatment
Active medical intervention in varicose veins can be divided into surgical and non-surgical treatments. Some doctors favor traditional open surgery, while others prefer the newer methods. Newer methods for treating varicose veins such as Endovenous Thermal Ablation (endovenous laser treatment or radiofrequency ablation), and foam sclerotherapy are not as well studied, especially in the longer term.
Surgical
Several techniques have been performed for over a century, from the more invasive saphenous stripping, to less invasive procedures like ambulatory phlebectomy and CHIVA.
Stripping
Stripping consists of removal of all or part the saphenous vein main trunk. The complications include deep vein thrombosis (5.3%), pulmonary embolism (0.06%), and wound complications including infection (2.2%). For traditional surgery, reported recurrence rates, which have been tracked for 10 years, range from 5-60%. In addition, since stripping removes the saphenous main trunks, they are no longer available for venous bypass in the future (coronary and/or leg artery vital disease)
CHIVA
CHIVA is an acronym from the scientific paper "Conservatrice et Hémodynamique de l'Insuffisance Veineuse en Ambulatoire" published in France in 1988. CHIVA relies on an hemodynamic impairment assessed by data and evidences depicted through ultrasound dynamic venous investigations. According to this new concept, the clinical symptoms of venous insufficiency are not the cause but the consequence of various abnormalities of the venous system. For example, a varicose vein being overloaded, may be dilated not only because of valvular incompetence (the most frequent) but because of a venous block (thombosis) or arterio-venous fistulae and so the treatment has to be tailored according the hemodynamic features. It generally consists in 1 to 4 small incisions under local anaesthesia in order to disconnect the varicose veins from the abnormal flow due to valvular incompetence which dilates them. The patient is dismissed the same day. This method leads to an improvement of the venous function, i.e oedema reduction, ulcer and other trophic disorder healing and varicose veins calibre reduction . and CHIVA vs Compression in Venous Ulcer treatment whilst preserving more superficial veins for their possible use in coronary or leg artery by-pass. The first available publication of CHIVA outcomes that meets current methodological standards is a study by Carandina et al., where a long term (10 years) randomized trial of CHIVA vs stripping was restricted to Shunt I varicose configurations ( 30-35% of the varicose configurations) . This is the reason as to why the authors estimate that only 30-35% of patients with varicose veins can be treated with CHIVA despite there being some bias in the selection of patients favoring CHIVA. This study showed that there were recurrent varices in 18% of cases treated by CHIVA vs 38% treated by stripping. Fortunately, Lurie’s statement has been contradicted by a subsequent randomized controlled trial published by Pares and al. in "Annals of Surgery" April 2010, a new Randomized Control Trial has been published, comparing Stripping Versus the CHIVA Method, showing efficiency of the latter compared with the standard stripping method, where all varicose veins configuration where included and “clinical outcomes in the CHIVA group were better (44.3% cure, 24.6% improvement, 31.1% failure) than in both the stripping with clinic marking (21.0% cure, 26.3% improvement,52.7% failure) and stripping with duplex marking (29.3% cure, 22.8% improvement, 47.9% failure) groups”. In addition to Carandina and Pares studies, two randomized trial , CHIVA vs stripping on varicose veins regarding immediate outcomes and CHIVA and CHIVA vs Compression in Venous Ulcer treatment make CHIVA the most rated therapeutic method in terms of Evidence Based Medicine. In "Annals of Surgery" April 2010, a new Randomized Control Trial has been published, comparing Stripping Versus the CHIVA Method, showing efficiency of the latter compared with the standard stripping method.
Other surgical treatments are:
- Ambulatory phlebectomy
- Vein ligation
- Cryosurgery- A cryoprobe is passed down the long saphenous vein following saphenofemoral ligation. Then the probe is cooled with NO2 or CO2 to a temperature of -850. The vein freezes to the probe and can be retrogradely stripped after 5 sec of freezing.It is a variant of Strippling. The only point of this technique is to avoid a distal incision to remove the stripper.
The American College of Phlebology (ACP) is a professional organization of physicians and allied health professionals that treat venous disease. Their membership spans 7 continents and 38 countries. To find a provider in your area visit www.phlebology.org or www.healthyveins.org
Non-surgical treatment
SCLEROTHERAPY
A commonly performed non-surgical treatment for varicose and "spider" leg veins is sclerotherapy in which medicine is injected into the veins to make them shrink. The medicines that are commonly used as sclerosants are polidocanol (POL), sodium tetradecyl sulphate (STS), Sclerodex (Canada), Hypertonic Saline, Glycerin and Chromated Glycerin. STS and Polidocanol(branded Asclera in the United States) liquids can be mixed with air or CO2 or O2 to create foams. Sclerotherapy has been used in the treatment of varicose veins for over 150 years. Sclerotherapy is often used for telangiectasias (spider veins) and varicose veins that persist or recur after vein stripping. Sclerotherapy can also be performed using foamed sclerosants under ultrasound guidance to treat larger varicose veins, including the great saphenous and small saphenous veins. A study by Kanter and Thibault in 1996 reported a 76% success rate at 24 months in treating saphenofemoral junction and great saphenous vein incompetence with STS 3% solution. A Cochrane Collaboration review concluded sclerotherapy was better than surgery in the short term (1 year) for its treatment success, complication rate and cost, but surgery was better after 5 years, although the research is weak. A Health Technology Assessment found that sclerotherapy provided less benefit than surgery, but is likely to provide a small benefit in varicose veins without reflux. This Health Technology Assessment monograph includes reviews of the epidemiology, assessment, and treatment of varicose veins, as well as a study on clinical and cost effectiveness of surgery and sclerotherapy. Complications of sclerotherapy are rare but can include blood clots and ulceration. Anaphylactic reactions are "extraordinarily rare but can be life-threatening," and doctors should have resuscitation equipment ready. There has been one reported case of stroke after ultrasound guided sclerotherapy when an unusually large dose of sclerosant foam was injected.
Endovenous thermal ablation
The Australian Medical Services Advisory Committee (MSAC) in 2008 has determined that endovenous laser treatment/ablation (ELA) for varicose veins "appears to be more effective in the short term, and at least as effective overall, as the comparative procedure of junction ligation and vein stripping for the treatment of varicose veins." It also found in its assessment of available literature, that "occurrence rates of more severe complications such as DVT, nerve injury and paraesthesia, post-operative infections and haematomas, appears to be greater after ligation and stripping than after EVLT". Complications for ELA include minor skin burns (0.4%) and temporary paraesthesia (2.1%). The longest study of endovenous laser ablation is 39 months.
Two prospective randomized trials found speedier recovery and fewer complications after radiofrequency ablation (ERA) compared to open surgery. Myers wrote that open surgery for small saphenous vein reflux is obsolete. Myers said these veins should be treated with endovenous techniques, citing high recurrence rates after surgical management, and risk of nerve damage up to 15%. In comparison, ERA has been shown to control 80% of cases of small saphenous vein reflux at 4 years, said Myers. Complications for ERA include burns, paraesthesia, clinical phlebitis, and slightly higher rates of deep vein thrombosis (0.57%) and pulmonary embolism (0.17%).One 3-year study compared ERA, with a recurrence rate of 33%, to open surgery, which had a recurrence rate of 23%.
ELA and ERA require specialized training for doctors and expensive equipment. ELA is performed as an outpatient procedure and does not require the use of an operating theatre, nor does the patient need a general anaesthetic. Doctors must use high frequency ultrasound during the procedure to visualize the anatomical relationships between the saphenous structures. Some practitioners also perform phlebectomy or ultrasound guided sclerotherapy at the time of endovenous treatment. Follow-up treatment to smaller branch varicose veins is often needed in the weeks or months after the initial procedure.
The American College of Phlebology (ACP) is a professional organization of physicians and allied health professionals that treat venous disease. Their membership spans 7 continents and 38 countries. To find a provider in your area visit www.phlebology.org or www.healthyveins.org more on wikipedia...















